Now Accepting New Patients!
We are currently accepting individuals ages 15+ who have been diagnosed with a Major Depressive Disorder.
Ready to get started with FSU Neuromodulation™?
Appointments can be made directly with the office by calling
850-644-5600
For referring physician offices: Physician Referral Form
Please fax the completed form back to 833-324-1669
Or, complete a referral online
Online Referral

Billing Options
We are currently participating with the following insurances: Aetna, Blue Cross Blue Shield, CHP, Cigna, Medicare, Optum/United Health Care, Optum VA Community Care Plan, and WellCare.
Pricing and approval will be dependent on your insurance provider. If your insurance is not listed or you do not have insurance, we also have self-pay options.
To make a payment on an existing patient account, please click below:
The TMS Treatment Process
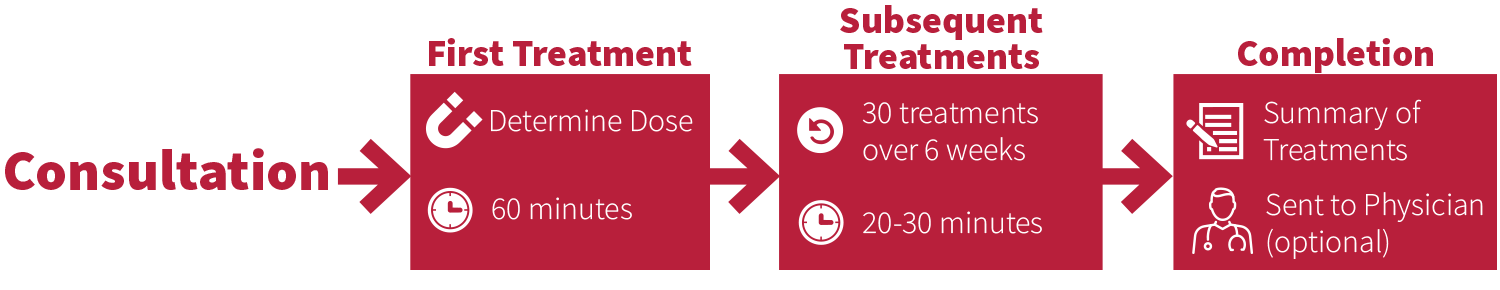
Step 1: Initial Consultation
Your clinician will refer you to our office for an initial consultation, during which you'll receive a Patient Intake Packet via email. This packet must be completed before your evaluation. If you have questions, call 850-644-5600. Once the packet is submitted, your appointment will be confirmed.
During the consultation, you'll complete additional paperwork and see a psychiatrist to determine if TMS is appropriate for you. Risks, benefits, and any questions will be addressed. If suitable for treatment and you wish to proceed, you will be scheduled for TMS once your insurance approves or you sign a payment plan agreement.
Step 2: First Treatment
The process begins with determining the appropriate dose of TMS, known as the "Motor Threshold," by placing the treatment coil gently on the scalp over the motor cortex to test various doses. This initial step takes about 30 minutes and is typically only done before the first treatment unless significant clinical changes occur.
For the treatment, the coil is positioned on the front of the head, marked by head measurements on a cap, producing clicking sounds as it delivers magnetic pulses. The treatment itself lasts 10 to 20 minutes, with no post-treatment restrictions. The first visit is approximately 60 minutes long.
Step 3: Subsequent Treatments
Before each treatment, you will be asked about any medical or psychiatric changes. You will receive earplugs, and the treatment coil will be placed on the front of your head for a 10-20 minute session. You can leave without restrictions afterwards, with visits lasting around 20-40 minutes.
After five treatments, you will complete a 15-minute questionnaire to monitor progress, which your physician will review. The initial course typically involves 30 treatments over six weeks, followed by 6 tapering sessions over three weeks.
Step 4: Completion
Once treatment is completed, a summary of your treatments received, and clinical progress can be sent to your physician if requested.
Optional: Preservation Treatments
Preservation treatments (at additional cost) may be required in the future depending upon your individual needs. You or your treating provider can contact us if preservation treatment is required.
Frequently Asked Questions
Will TMS be Helpful for Me?
Although we cannot guarantee symptom improvement, TMS is cleared by the FDA for treatment of Major Depressive Disorder. Numerous studies have demonstrated the safety and efficacy of TMS for depression - even for patients with Treatment Resistant Depression.
How Does TMS Work?
For more information on how TMS works, please visit our Services page.
Can I Stay on My Medications During Treatment?
Most medications are safe to take while undergoing TMS treatment, however, there are some medications that need to be stopped prior to starting TMS. Be sure to have a list of your current medications for your consult. We ask that you avoid any medication changes during the TMS treatment course.
Am I Required to Make Any Lifestyle Changes During Treatment?
TMS has no cognitive side effects and does not require anesthesia or any restriction of activities, so you are encouraged to continue your regular schedule. We do ask that you refrain form heavy alcohol use (>2 drinks per day) and not use any recreational drugs during the treatment period.
Are There Any Side Effects or Risks to Treatment?
There are no cognitive side effects from TMS treatment or any restrictions on activities. The most common physical side effects are headache, scalp discomfort during treatment, and fatigue. There is an extremely rare risk of seizure (less than 1 in 1,000 patients) that we mitigate through screening and evaluations prior to beginning treatment.
How Does TMS Feel?
Our participants and patients most commonly say that the pulses feel like a tapping or mild electrical sensation depending on the treatment type.